Clinical testing found the vaccine outperforms Oxford/AstraZeneca’s.
The vaccine, now called SKYCovione, is the world’s first computationally designed protein medicine.
University of Washington to waive royalty fees for the duration of the pandemic.
A vaccine for COVID-19 developed at the University of Washington School of Medicine has been approved by the Korean Ministry of Food and Drug Safety for use in adults. The vaccine, now under the brand name SKYCovione, was found to be more effective than the Oxford/AstraZeneca vaccine sold under the brand names Covishield and Vaxzevria.
Update (2023): SKYCovione was also approved in the U.K. and granted an Emergency Use Listing by the WHO.
The Seattle scientists behind the new vaccine sought to create a ‘second-generation’ COVID-19 vaccine that is safe, effective at low doses, simple to manufacture, and stable without deep freezing. These attributes could enable vaccination at a global scale by reaching people in areas where medical, transportation, and storage resources are limited. The South Korean company SK Bioscience is leading the vaccine’s clinical development abroad.
“We know more than two billion people worldwide have not received a single dose of vaccine,” said David Veesler, an associate professor of biochemistry at UW School of Medicine and co-developer of the vaccine. “If our vaccine is distributed through COVAX, it will allow it to reach people who need access.”
The University of Washington is licensing the vaccine technology royalty-free for the duration of the pandemic.
How the vaccine works
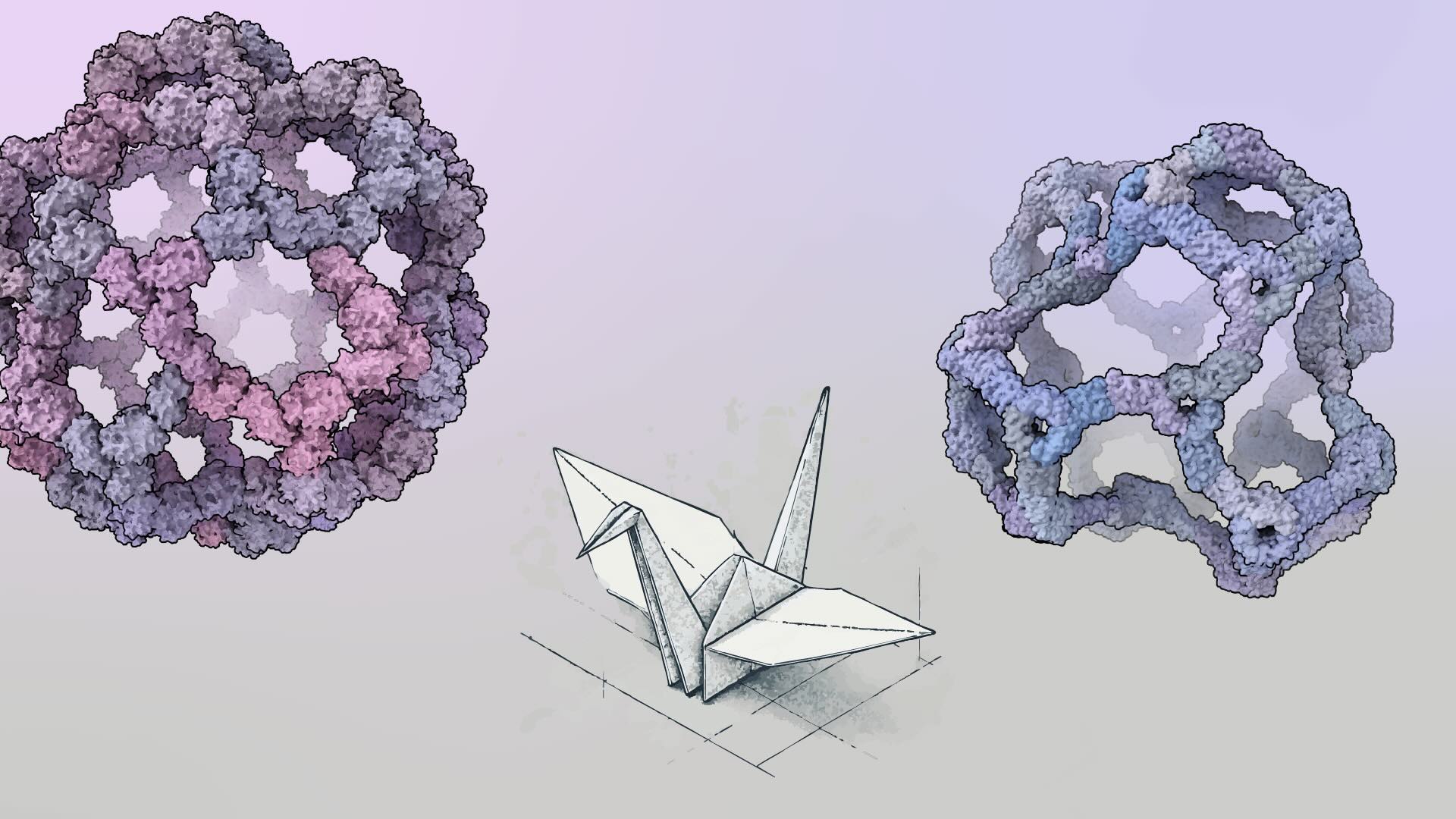
Unlike the earliest approved vaccines for COVID-19 that make use of mRNA, viral vectors, or an inactivated virus, SKYCovione is made of proteins that form tiny particles studded with fragments of the pandemic coronavirus. These nanoparticles were designed by scientists at UW Medicine and advanced into clinical trials by SK Bioscience and GlaxoSmithKline with financial support from the Coalition for Epidemic Preparedness Innovations (CEPI). SKYCovione includes GlaxoSmithKline’s pandemic adjuvant AS03.
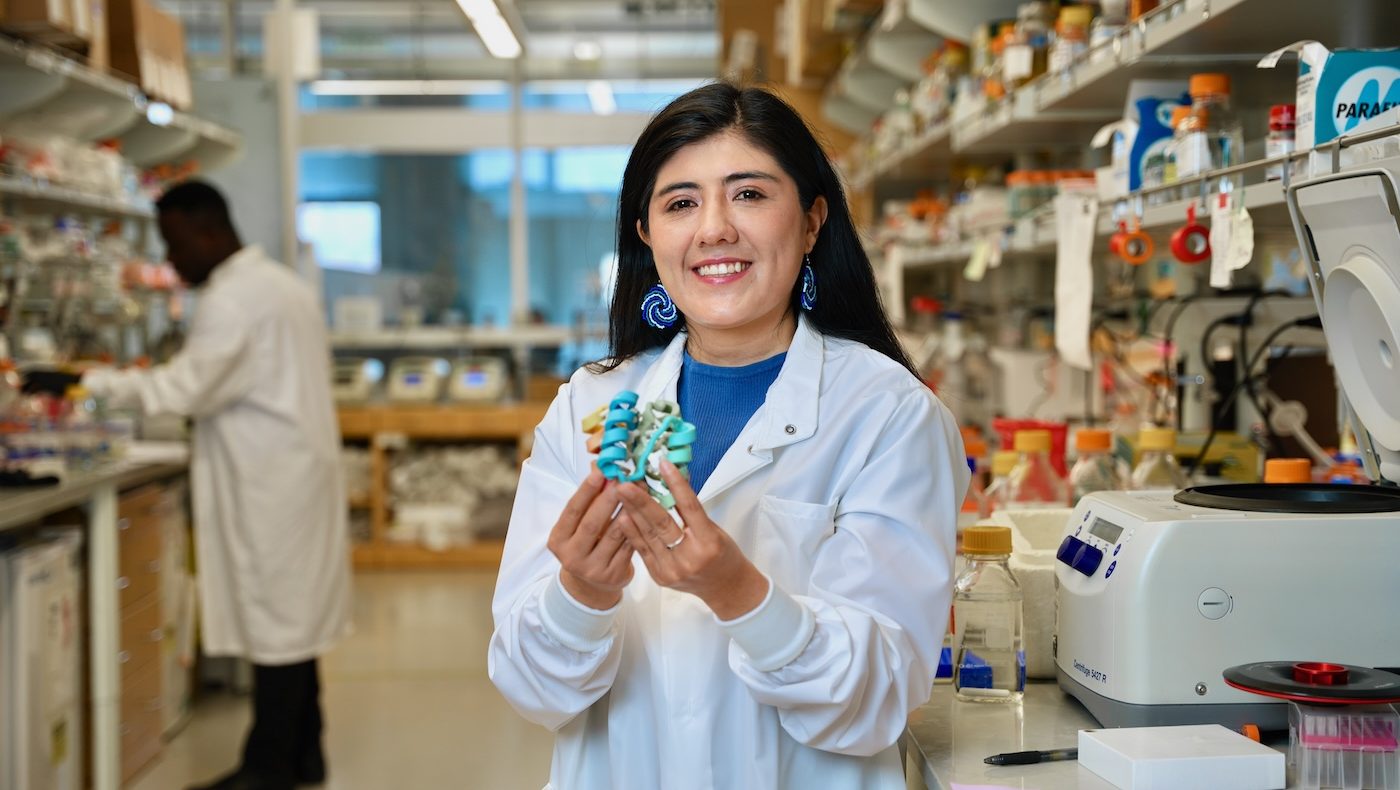
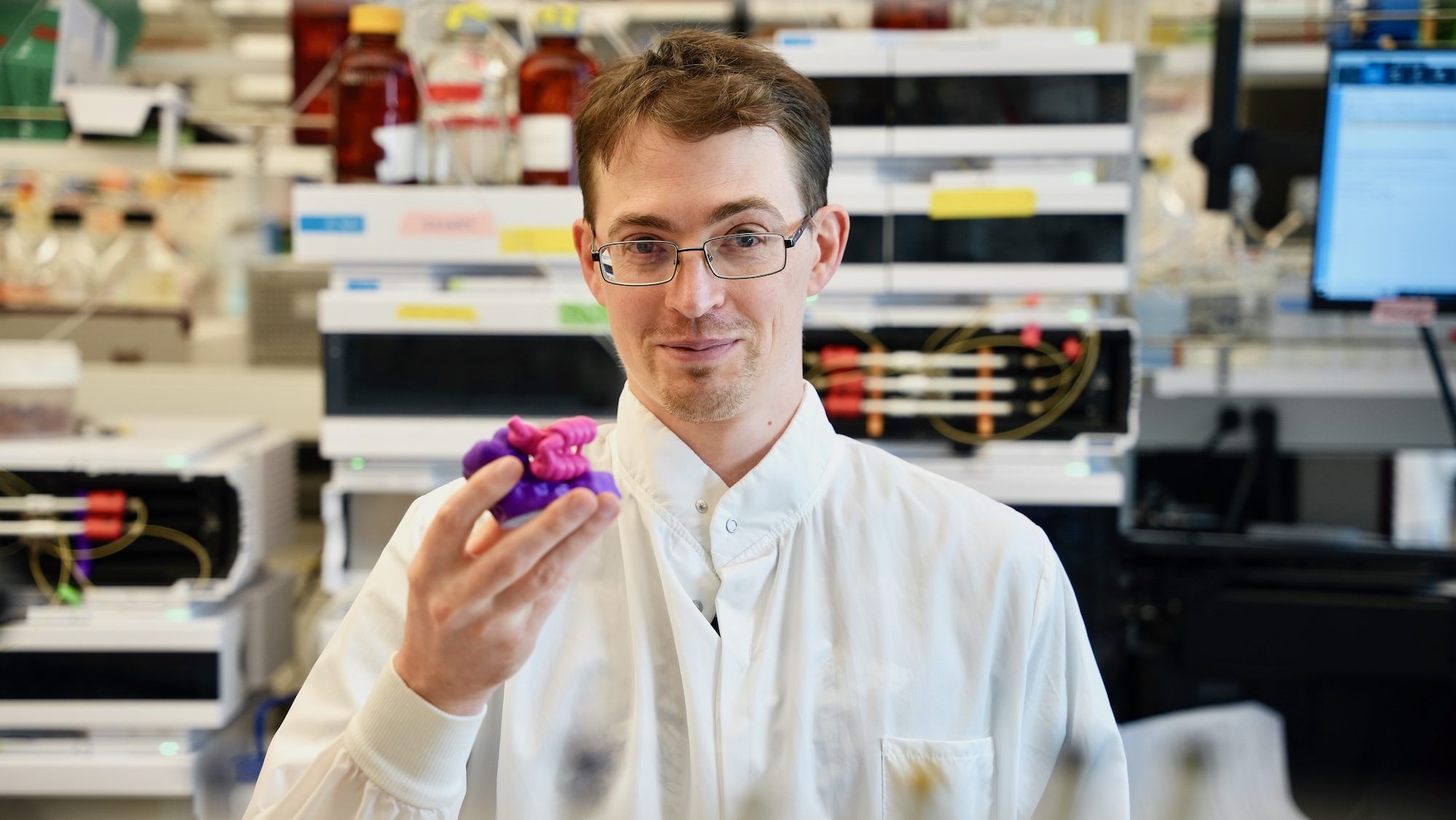
Two laboratories in the UW Medicine Department of Biochemistry led the initial development of the protein-based vaccine: the King Lab at the Institute for Protein Design pioneered the vaccine’s self-assembling protein nanoparticle technology while the Veesler Lab identified and integrated a key fragment of the SARS-CoV-2 Spike protein onto the nanoparticles.
“This vaccine was designed at the molecular level to present the immune system with a key part of the coronavirus spike protein. We know this part is targeted by the most potent antibodies,” explained Neil King, an assistant professor of biochemistry at UW Medicine and co-developer of the vaccine.


Clinical trial results
A multinational Phase 3 trial involving 4,037 adults over 18 years of age found that SKYCovione elicits roughly three times more neutralizing antibodies than the Oxford/AstraZeneca vaccine Covishield/Vaxzevria. In these studies, SKYCovione or Covishield/Vaxzevria was administered twice with an interval of four weeks.
In addition, the antibody conversion rate, which refers to the proportion of subjects whose virus-neutralizing antibody level increased fourfold or more after vaccination, was higher with SKYCovione. According to data collected by SK Bioscience, 98 percent of subjects achieved antibody conversion, compared to 87 percent for the control vaccine.
Among study participants 65 years of age or older, the antibody conversion rate of those vaccinated with SKYCovione was over 95 percent, which was a significant difference compared to the control vaccine (about 79 percent for the elderly), raising the expectation that SKYCovione can be used effectively to protect the elderly.
The Phase 3 trial also found that T cell activation levels, which help protect the body from COVID-19, were similar or higher with SKYCovione.
Phase 1/2 trial results announced by SK Bioscience last November and posted as a preprint found that SKYCovione was safe and produced virus-neutralizing antibodies in all trial participants receiving the adjuvanted vaccine. In the Phase 3 trial, there were again no serious adverse reactions to the vaccine.
Years in the making
David Veesler has been studying coronaviruses since 2015. Using advanced electron microscopes, researchers in his lab were the first to identify how the novel coronavirus enters human cells. They were also among the first to report detailed structural information about the SARS-CoV-2 Spike protein, a critical piece of the virus’ infectious machinery.
In 2016, scientists in the King Lab began developing a strategy for building a new type of vaccine. They created proteins that self-assemble into precise spherical particles and later showed that these nanoparticles could be decorated with proteins from a virus.
Researchers from the two labs worked together in the earliest months of the COVID-19 pandemic to design a protein nanoparticle decorated with 60 copies of the Spike protein’s receptor-binding domain. The designed nanostructure mimics the repetitive nature of proteins on the surface of viruses, a property that the immune system responds strongly to.
“In order to focus the antibody response where it matters most, we decided to include in the vaccine only the receptor-binding domain from the coronavirus Spike protein,” said Veesler. “We are thrilled to see that this strategy paid off and has led to a successful subunit vaccine.”
In initial animal studies reported in late 2020 in Cell, the nanoparticle vaccine was found to produce high levels of virus-neutralizing antibodies at low doses. These antibodies target several different sites on the coronavirus Spike protein, a desirable quality that may enhance protection against future coronavirus variants.
Further preclinical research published in Nature also showed that the vaccine conferred robust protection and produced a strong B-cell response in non-human primates. This may improve how long the protective effects of the vaccine last.
In a recent preprint, a third dose of the vaccine was found to confer strong protection against the Omicron variant of SARS-CoV-2 in animals. SK Bioscience plans to test third doses in human clinical trials soon.
The role of philanthropy
Development of the vaccine at UW Medicine was supported by the Bill & Melinda Gates Foundation, National Institutes of Health, Pew Charitable Trust, Burroughs Wellcome Fund, Fast Grants, and by gifts from Jodi Green and Mike Halperin, Nicolas and Leslie Hanauer, Rob Granieri, anonymous donors, and other granting agencies, including Open Philanthropy. Support leveraged via The Audacious Project was made possible through the generosity of Laura and John Arnold, Steve and Genevieve Jurvetson, Chris Larsen and Lyna Lam, Lyda Hill Philanthropies, Miguel McKelvey, the Clara Wu and Joe Tsai Foundation, Rosamund Zander and Hansjörg Wyss for the Wyss Foundation, and several anonymous donors.
SK Bioscience received support for clinical testing from the Bill & Melinda Gates Foundation and the Center for Epidemic Preparedness (CEPI), which is a global partnership supporting vaccine development to fight pandemics. CEPI, along with the World Health Organization and Gavi, the Vaccine Alliance, are co-leaders of COVAX.