Washington Research Foundation (WRF) has awarded a $250,000 phase 2 technology commercialization grant to Anindya Roy, Ph.D., to further develop a novel miniprotein binder for the treatment of idiopathic pulmonary fibrosis (IPF). Roy, an acting instructor in David Baker’s lab at the University of Washington’s Institute for Protein Design (IPD), is building on positive results from a WRF phase 1 grant.
IPF is a chronic progressive respiratory disease with uncertain causes and no cure. It produces scarring in the lungs, resulting in severe breathlessness, fatigue and heart failure. Patients typically survive for less than five years from diagnosis. Current drug therapies can improve overall quality of life for patients with mild-to-moderate IPF, but do not have any effect on overall survival. Moreover, the side effects associated with current therapies can be debilitating, and include diarrhea, nausea and impaired liver function. Lung transplants, the only option to improve an IPF patient’s overall respiratory health, are risky and expensive. There is therefore a clear need for better therapeutics to treat this disease.
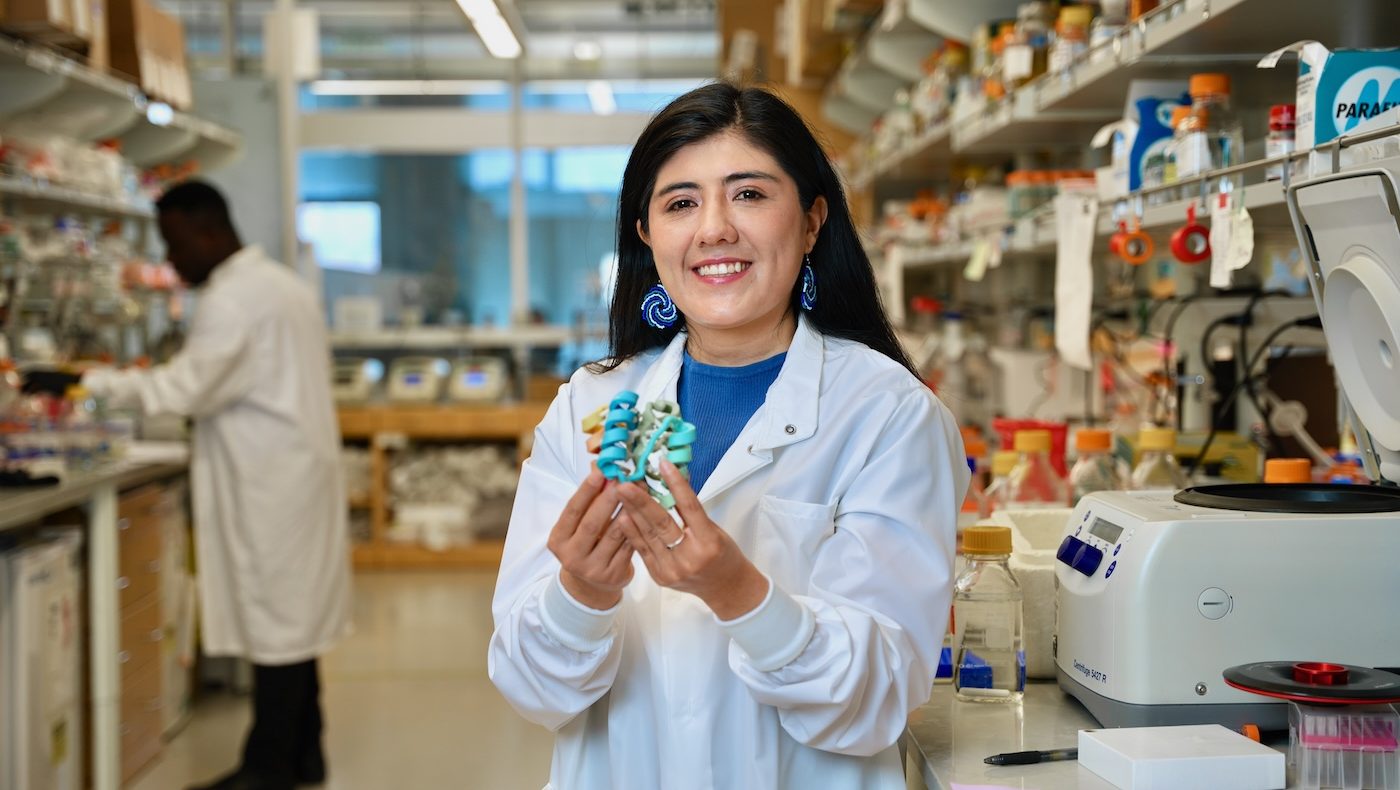
As a WRF Innovation Postdoctoral Fellow hired with the assistance of a $31.2 million pledge from WRF to the University of Washington in 2014, Roy designed a miniprotein that binds to the αvβ6 integrin, a cell-surface receptor that promotes fibrosis. αvβ6 has also been identified as a likely contributor to lung damage in patients infected during the severe acute respiratory syndrome (SARS) outbreak in 2003 and is believed to be linked to similar issues in COVID-19 patients. There is evidence that αvβ6 promotes cancers of the lung and other organs.
Other therapies that target αvβ6 are also being developed, but Roy’s inhibitor protein has several advantages that make it a particularly promising therapeutic candidate. The binding to αvβ6 is highly specific, and the miniprotein is also extremely stable, making it particularly suitable for nebulization and delivery as an inhaled therapeutic that can directly target the lungs. WRF provided an $80,000 phase 1 technology commercialization grant in 2019 to enable Roy and his colleagues to initially explore the binder’s potential for therapeutic use against IPF. In vivo tests in mouse models indicated that the miniprotein can be injected to reduce lung fibrosis and improve lung function. The phase 2 funding will seek to generate further data to demonstrate the safety and efficacy of the minibinder as a potential therapeutic, and show that it can be delivered via inhalation.
“Advancing this miniprotein as a potential therapeutic is exactly the type of work that WRF believes will have a genuine impact on human health,” said Meher Antia, Ph.D., director of grant programs at WRF. “With limited options for treating a disease that causes much suffering, the work that Anindya and the IPD team is doing is extremely important and we are delighted to continue to support it.”
“The latest funding from WRF will enable us to reach several major milestones,” said Roy. “We’ll be conducting mouse-model studies to determine the ideal delivery method—which we expect will be through a nebulizer—and measure toxicity to establish optimal dosing. Our unique capabilities to design hyperstable miniproteins give us a competitive advantage over other biologics for a wide variety of pulmonary diseases.”
About Washington Research Foundation:
Washington Research Foundation (WRF) supports research and scholarship in Washington state, with a focus on life sciences and enabling technologies. Learn more at wrfseattle.org